Discover Advantages of Deep Brain Stimulation Therapy
Deep Brain Stimulation (DBS) offers transformative benefits for individuals grappling with neurological disorders, providing an innovative and controlled approach to managing symptoms that were once thought unmanageable. Understanding the DBS benefits in detail can further illuminate its impact on patients’ lives.
"*" indicates required fields
Whereas many practitioners of DBS often lack specialized training and the diversity of options for their patients, Dr. Taghva stands distinctively ahead. He has not only performed hundreds of DBS implants for Parkinson’s Disease and Essential Tremor but was also the pioneering neurosurgeon in Orange County to introduce DBS for epilepsy.
Dr. Taghva is well-versed with and routinely implants devices from prominent manufacturers like Abbott, Boston Scientific, and Medtronic (Medtronic DBS). His vast experience empowers him to assist patients in choosing the ideal device tailored to their needs. A fervent advocate for “directional lead placement,” Dr. Taghva employs highly specialized DBS leads that can steer electrical stimulation, resulting in superior outcomes for his patients, minimizing side effects.
In a groundbreaking advancement, Dr. Taghva introduced the “single-stage, asleep DBS” in Orange County. Traditionally, DBS demanded 2 or 3 separate surgical stages. In contrast, Dr. Taghva’s method integrates both lead placements and battery installation in one comprehensive procedure under general anesthesia. This not only enhances patient comfort but also allows them to return home the very next day.
Supporting the efficacy of this approach, the 2018 article titled “Clinical outcomes following awake and asleep deep brain stimulation for Parkinson disease” published in the Journal of Neurosurgery by Chen et al found that clinical outcomes between awake and asleep DBS are comparably effective. However, patients undergoing asleep DBS reported elevated comfort levels, and the procedure’s advantage lies in its single-stage completion.
Further enhancing his reputation in the field, Dr. Taghva is Orange County’s premier implanter of “asleep” DBS for Parkinson’s disease. This approach uses sophisticated intraoperative imaging and ensures patients are at ease under anesthesia, while still using complex brain recording techniques such as microelectrode recording (MER) to further refine electrode placement. The amalgamation of these techniques under Dr. Taghva’s expert hands has proven more accurate in DBS placement compared to the traditional awake lead placement procedures.
Dr. Taghva’s dedication to his craft is reflected in the joy and satisfaction of his DBS patients. They stand as regional advocates for the therapy. Leading publications, like Health Matters, regularly spotlight his patients, heralding them as DBS success stories. Both Medicare and most private insurances recognize and cover DBS treatments under his care.
A product of elite institutions, Dr. Taghva earned his medical degree from the esteemed Johns Hopkins University School of Medicine. He further refined his skills during his residency at the University of Southern California, followed by a specialized fellowship at The Ohio State University. As a board-certified neurosurgeon, Dr. Taghva’s excellence hasn’t gone unnoticed. For six consecutive years, his peers have honored him as an Orange County Physician of Excellence, and he has earned the accolade of a Super Doctors Rising Star.
Alexander Taghva, M.D., F.A.A.N.S., in Mission Viejo, CA, offers DBS, a unique surgical treatment, targeting problematic brain impulses directly. Those unresponsive to conventional treatments for conditions like Parkinson’s Disease or Essential Tremor may find a beacon of hope in this transformative procedure under Dr. Taghva’s expert guidance.
Call today to schedule your consultation
What is Deep Brain Stimulation?
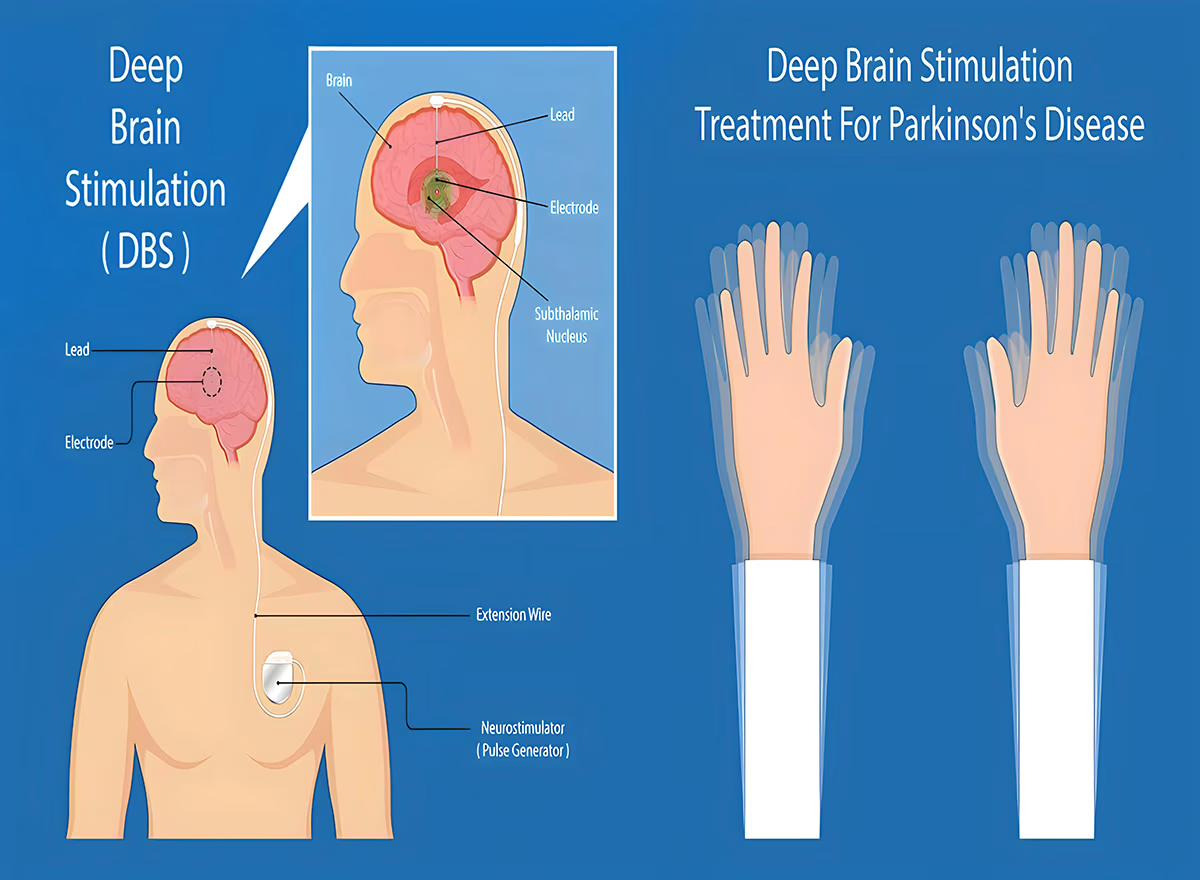
DBS is a form of neurosurgery that treats certain medical problems by providing electrical stimulation to a specific region of brain tissue. The method, often referred to as a “pacemaker for the brain,” usually occurs over two different operations.
During DBS surgery, a stimulator device system is inserted into the brain through a small opening in the skull. The surgeon is guided with a type of imaging provided by magnetic resonance imaging (MRI), CT scanning, or a computer program. Dr. Taghva implants wire electrodes into the side of the brain on both the left and right, targeting parts of the brain where abnormal nerve signals are generated, creating a roadmap of your brain with images obtained from MRI. The electrodes are held in place by small disks that are secured on top of the brain.
At a later date, wire leads are connected to the electrodes and placed below the skin, following the curvature of the head and neck. There is a connection between the wires and a pulse generator in the chest wall below the collarbone.
Local anesthesia is an option for patients who want to stay conscious during the procedure. This allows neurosurgeons to observe the real-time effects of their surgery; however, since the brain has no pain receptors, some neurosurgeons choose to perform a different version of DBS surgery while patients are fully asleep.
Three to six weeks later, patients will return to the operating room to undergo the placement of the pulse generator. The surgeon will typically complete this procedure on an outpatient basis. During another appointment, the surgeon programs the patient’s DBS system to deliver the type of electrical signals that will be most beneficial for the patient’s condition.
When will you need Deep Brain Stimulation?
The FDA has granted approval for DBS as an effective treatment option after successful clinical trials for various neurological disorders which can have a major impact on patient’s lives:
- Parkinson’s disease and essential tremor – 1997
- Dystonia – 2003
- Obsessive-compulsive disorder – 2009
- Epilepsy – 2018
For those who have not had positive outcomes from other forms of treatment and for whom symptoms are greatly impacting their day-to-day life, DBS surgery is a suitable option. DBS offers relief from these symptoms, delivering electrical stimulation to the interfering brain cells without causing the side effects associated with medication.
Researchers are currently exploring the potential of DBS to treat various other medical issues, such as multiple sclerosis, and psychological treatments, like major depression. It is possible that in the future, DBS will be an effective option for these conditions.
Testimonials
Who is a Candidate for Deep Brain Stimulation?
Dr. Taghva examines everyone to determine the most suitable treatment course for them. Typically, candidates for DBS in Mission Viejo fall within two types: patients with movement disorder symptoms or mental health problems.
A range of movement disorders results from a neurological issue like Parkinson’s disease, which creates involuntary movement and motor symptoms that disrupt a patient’s regular abilities and daily activities. Parkinson’s disease symptoms include tremors, bradykinesia (slower-than-normal movements), muscle rigidity, and poor balance or posture.
A patient’s quality of life diminishes significantly when they show uncontrolled movement. DBS of the globus pallidus internus or subthalamic nucleus can treat isolated dystonia (uncontrolled muscle contractions) with or without tremors and with no additional neurological issues.
Certain neuropsychiatric conditions, such as obsessive-compulsive disorder (OCD) and Tourette syndrome, can manifest as mental disorders originating from the nervous system. Electrical impulses help to manage symptoms associated with these disorders.
Those with dementia and severe untreated depression are not candidates for DBS in Dr. Taghva’s Mission Viejo practice. DBS can worsen memory problems and lead to suicidal ideation. After treating depression, surgery may be a good treatment option.
A Deep Brain Stimulation Consultation
In his private consultation with patients in Mission Viejo, CA, Dr. Taghva thoroughly evaluates each case to determine if DBS or an alternative treatment is the best option for complete pain relief. He will recommend this advanced surgical procedure for individuals whose symptoms of an approved DBS condition are moderate to severe, who have tried other treatments that were not successful, and who would benefit from fewer side effects from medications. Qualifying patients must also meet the general requirements for being viable candidates for surgery.
The DBS consultation is lengthier than other procedures because preoperative evaluations are typically conducted as a series of tests. In many cases, patients may need to be evaluated both on and off their medications. Because DBS can treat numerous conditions, the prerequisites for surgery will differ from one patient to the next. Assessment may involve consulting with several healthcare providers.
During a consultation with Dr. Taghva, the neurosurgeon works with the patient to prepare an optimal treatment plan. In some cases, the recommendation may include DBS surgery.
Are you ready to meet a leading Orange County Neurosurgeon?
Preparing for Deep Brain Stimulation Surgery
DBS in Orange County may require a series of tests prior to treatment. Your physician will recommend you cease any medications for the duration of testing. If discontinuing medications isn’t an option, sedation DBS may be a feasible solution.
DBS candidates should have a physical exam conducted by their primary care physician, blood tests, an electrocardiogram (EKG), and a chest X-ray. This helps Dr. Taghva determine that the patient is healthy enough for the procedure. Before the procedure, you should discuss chronic illnesses and related medications.
The Day of Deep Brain Stimulation Surgery
Patients are typically awake during DBS surgery in Orange County. However, there is a newer technique while the patient is asleep during the procedure.
The doctor carefully puts on a frame to the head of the patient, who is conscious yet calm so that they can perform surgery. Dr. Taghva administers topical anesthetic (numbing) as pins penetrate the forehead and the posterior of the skull with the framing device. With this frame in place, patients will have an MRI, or CT scan revealed for Dr. Taghva and his surgical team to observe the brain in correlation with pin placement in the frame.
Computerized equipment, a mobile X-ray unit, and a robot ensure the accurate placement of the electrodes in the brain. Different pieces of equipment, like an arc, can be fitted to the frame on the head to aid precision.
Once the electrodes are in place, the surgeon will activate the deep brain stimulator system. Dr. Taghva will be able to view symptom changes and any side effects while adjusting the impulses. After the placement of the electrodes, there will be more captured images to confirm proper placement.
The surgeon performs DBS while the patient is fully asleep. The procedure begins inside an MRI machine, which provides real-time visualization. While X-rays take still snapshots of the brain and can offer image guidance on the area before and after each change, an MRI provides continuous imaging to check brain performance.
An aiming device is placed on the scalp, which enables visibility and adjustments to be made while the patient is in the MRI machine. The deep brain stimulation device creates points that will show up on computerized equipment. This allows the neurosurgeon to plot the correct points for electrode placement.
Deep Brain Stimulation Recovery
After DBS, patients will undergo a healing process that is unique to their situation.
After surgery, patients may experience slight discomfort in the area of their incision and pin sites where the doctor administered anesthesia. However, since the brain has no pain receptors, it will not feel pain. To ensure your comfort during this process, Dr. Taghva will provide you with the necessary pain medications before your operation.
Patients may also feel some discomfort at the site of the pulse generator for a period of time. With an adjusted medication regimen and the initial programming of the stimulator device, patients may notice different sensations or muscle involuntary movements.
Four to six weeks postoperatively, the team can begin programming the system. It can take a few to several months to adjust the settings of the DBS generator for the best results. Patients must adhere to any restrictions provided by Dr. Taghva for the safest recovery and best results.

Tips To Keep Your DBS Recovery On Track
The following are some ways to keep your brain surgery rehabilitation on the right track. Depending on your specific recovery plan, you will benefit in different ways.
1
Attend your DBS follow-up appointments
Your neurosurgeon will likely want to see you in various increments after your surgery. Be sure to make these appointments a priority. Your doctor will use these to catch any issues and recommend further action.
2
Ask for help during your DBS recovery
Over 1.5 billion individuals suffer from a chronic pain condition. However, they should not have to go through this on their own. If your body cannot carry out particular tasks due to physical discomfort, do not be afraid to seek assistance.
3
Follow your DBS specialist’s instructions
You may attend physical therapy or see a speech-language pathologist following your surgery. If they give you exercises to perform at home, be sure to stick with these. Your progress may depend on it.
4
Be patient
Even after this minimally-invasive procedure, patients may take time to heal. Know that progress will come, and be patient with your body.
5
Call your doctor about post-DBS issues
If you experience seizures, chronic pain symptoms, numbness, or other neurological complications, call 911 or your doctor immediately. This depends on the severity of the situation.
What Are the Possible Side Effects or Risks of DBS Surgery?
While Dr. Taghva takes every precaution possible, DBS has inherent risks. Patients can discuss any concerns about this treatment at Orange County Neurological Associates with Dr. Taghva during their consultation. Deep brain stimulation risks may include:
| Stroke | Hemorrhage | DBS system malfunctions |
| Adverse effects of stimulation | Worsening memory | Suicidal ideation |

Why Choose Dr. Alexander Taghva
Dr. Alexander Taghva is a leading board-certified neurosurgeon, specializing in brain surgery, endoscopic spine surgery, as well as spine disorders. Also, he is the only spine surgeon in Orange County and southern California who offers endoscopic laminotomy surgery. Dr. Taghva:
- Graduated from John Hopkins University School of Medicine and completed his residency at the University of California
- Completed a prestigious fellowship at The Ohio State University in Neuromodulation and Functional Neurosurgery
- Specializes in minimally invasive and endoscopic surgery, spinal stenosis, artificial disc replacement, spinal disorders, spinal surgery revision, and other spinal conditions.
- Specializes in brain surgery to treat trigeminal neuralgia, brain tumors, pituitary tumors, and Parkinson’s disease.
- A highly-respected neurosurgeon with many years of experience, including treating chronic pain via stimulation of the spinal cord and brain
- Actively involved in medical research and the lead investigator for clinical trials on spinal cord stimulation